Analgesic nephropathy

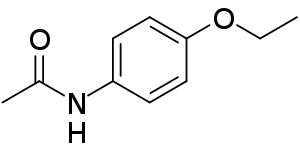
Analgesic nephropathy is injury to the kidneys caused by analgesic medications such as aspirin, phenacetin, and paracetamol. The term usually refers to damage induced by excessive use of combinations of these medications, especially combinations that include phenacetin. It may also be used to describe kidney injury from any single analgesic medication. Analgesic nephropathy is injury to the kidneys caused by analgesic medications such as aspirin, phenacetin, and paracetamol. The term usually refers to damage induced by excessive use of combinations of these medications, especially combinations that include phenacetin. It may also be used to describe kidney injury from any single analgesic medication. The specific kidney injuries induced by analgesics are renal papillary necrosis and chronic interstitial nephritis. They appear to result from decreased blood flow to the kidney, rapid consumption of antioxidants, and subsequent oxidative damage to the kidney. This kidney damage may lead to progressive chronic kidney failure, abnormal urinalysis results, high blood pressure, and anemia. A small proportion of individuals with analgesic nephropathy may develop end-stage kidney disease. Analgesic nephropathy was once a common cause of kidney injury and end-stage kidney disease in parts of Europe, Australia, and the United States. In most areas, its incidence has declined sharply since the use of phenacetin fell in the 1970s and 1980s. Common findings in people with analgesic nephropathy include headache, anemia, high blood pressure (hypertension), and white blood cells in the urine (pyuria). Some individuals with analgesic nephropathy may also have protein in their urine (proteinuria). Complications of analgesic nephropathy include pyelonephritis and end-stage kidney disease. Risk factors for poor prognosis include recurrent urinary tract infection and persistently elevated blood pressure. Analgesic nephropathy also appears to increase the risk of developing cancers of the urinary system. The scarring of the small blood vessels, called capillary sclerosis, is the initial lesion of analgesic nephropathy. Found in the renal pelvis, ureter, and capillaries supplying the nephrons, capillary sclerosis is thought to lead to renal papillary necrosis and, in turn, chronic interstitial nephritis. How phenacetin and other analgesics lead to this damage is incompletely understood. It is currently thought that the kidney toxicities of NSAIDs and the antipyretics phenacetin and paracetamol may combine to give rise to analgesic nephropathy. A committee of investigators reported in 2000 that there was insufficient evidence to suggest that non-phenacetin analgesics by themselves are associated with analgesic nephropathy. Proper kidney function depends upon adequate blood flow to the kidney. Kidney blood flow is a complex, tightly regulated process that relies on a number of hormones and other small molecules, such as prostaglandins. Under normal circumstances, prostaglandin E2 (PGE2) produced by the kidney is necessary to support adequate blood flow to the kidney. Like all prostaglandins, PGE2 synthesis depends upon the cyclooxygenases. Aspirin and other NSAIDs are inhibitors of the cyclooxygenases. In the kidney, this inhibition results in decreased PGE2 concentration causing a reduction in blood flow. Because blood flow to the kidney first reaches the renal cortex (outside) and then the renal medulla (inside), the deeper structures of the kidney are most sensitive to decreased blood flow. Thus the innermost structures of the kidney, known as the renal papillae, are especially dependent on prostaglandin synthesis to maintain adequate blood flow. Inhibition of cyclooxygenases therefore rather selectively damages the renal papillae, increasing the risk of renal papillary necrosis.