Cat scratch

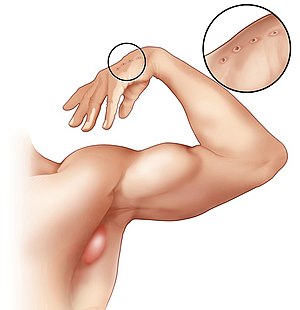
Cat-scratch disease (CSD) is an infectious disease that results from a scratch or bite of a cat. Symptoms typically include a non-painful bump or blister at the site of injury and painful and swollen lymph nodes. People may feel tired, have a headache, or a fever. Symptoms typically begin within 3-14 days following infection. Cat-scratch disease (CSD) is an infectious disease that results from a scratch or bite of a cat. Symptoms typically include a non-painful bump or blister at the site of injury and painful and swollen lymph nodes. People may feel tired, have a headache, or a fever. Symptoms typically begin within 3-14 days following infection. Cat-scratch disease is caused by the bacterium Bartonella henselae which is believed to be spread by the cat’s saliva. Young cats pose a greater risk than older cats. Occasionally dog scratches or bites may be involved. Diagnosis is generally based on symptoms. Confirmation is possible by blood tests. The primary treatment is supportive. Antibiotics speed healing and are recommended in those with severe disease or immune problems. Recovery typically occurs within 4 months but can require a year. About 1 in 10,000 people are affected. It is more common in children. Cat-scratch disease commonly presents as tender, swollen lymph nodes near the site of the inoculating bite or scratch or on the neck, and is usually limited to one side. This condition is referred to as regional lymphadenopathy and occurs 1–3 weeks after inoculation. Lymphadenopathy in CSD most commonly occurs in the arms, neck, or jaw, but may also occur near the groin or around the ear. A vesicle or an erythematous papule may form at the site of initial infection. Most patients also develop systemic symptoms such as malaise, decreased appetite, and aches. Other associated complaints include headache, chills, muscular pains, joint pains, arthritis, backache, and abdominal pain. It may take 7 to 14 days, or as long as two months, for symptoms to appear. Most cases are benign and self-limiting, but lymphadenopathy may persist for several months after other symptoms disappear. The disease usually resolves spontaneously, with or without treatment, in one month. In rare situations, CSD can lead to the development of serious neurologic or cardiac sequelae such as meningoencephalitis, encephalopathy, seizures, or endocarditis. Endocarditis associated with Bartonella infection has a particularly high mortality. Parinaud's oculoglandular syndrome is the most common ocular manifestation of CSD, and is a granulomatous conjunctivitis with concurrent swelling of the lymph node near the ear. Optic neuritis or neuroretinitis is one of the atypical presentations. People who are immunocompromised are susceptible to other conditions associated with B. henselae and B. quintana, such as bacillary angiomatosis or bacillary peliosis. Bacillary angiomatosis is primarily a vascular skin lesion that may extend to bone or be present in other areas of the body. In the typical scenario, the patient has HIV or another cause of severe immune dysfunction. Bacillary peliosis is caused by B. henselae that most often affects patients with HIV and other conditions causing severe immune compromise. The liver and spleen are primarily affected, with findings of blood-filled cystic spaces on pathology. Bartonella henselae is a fastidious, intracellular, Gram-negative bacterium. The cat was recognized as the natural reservoir of the disease in 1950 by Robert Debré. Kittens are more likely to carry the bacteria in their blood, so may be more likely to transmit the disease than adult cats. However, fleas serve as a vector for transmission of B. henselae among cats, and viable B. henselae are excreted in the feces of Ctenocephalides felis, the cat flea. Cats could be infected with B. henselae through intradermal inoculation using flea feces containing B. henselae. As a consequence, a likely means of transmission of B. henselae from cats to humans may be inoculation with flea feces containing B. henselae through a contaminated cat scratch wound or by cat saliva transmitted in a bite. Ticks can also act as vectors and occasionally transmit the bacteria to humans. Combined clinical and PCR-based research has shown that other organisms can transmit Bartonella, including spiders. Cryptic Bartonella infection may be a much larger problem than previously thought, constituting an unrecognized occupational health hazard of veterinarians. The Warthin–Starry stain can be helpful to show the presence of B. henselae, but is often difficult to interpret. B. henselae is difficult to culture and can take 2–6 weeks to incubate. The best diagnostic method available is polymerase chain reaction, which has a sensitivity of 43-76% and a specificity (in one study) of 100%.