Intracytoplasmic sperm injection

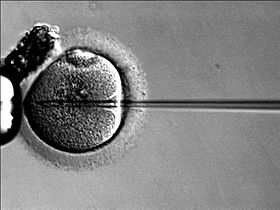
Intracytoplasmic sperm injection (ICSI /ˈɪksi/ IK-see) is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method acrosome reaction is skipped. Intracytoplasmic sperm injection (ICSI /ˈɪksi/ IK-see) is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method acrosome reaction is skipped. There are several differences within classic IVF and ICSI. However, the steps to be followed before and after insemination are the same. In terms of insemination, ICSI needs one only sperm cell per oocyte, meanwhile IVF needs between 50 and 100 thousands. This is due to the fact that in IVF acrosome reaction has to take place and thousands of sperm cells have to be involved. Once fertilized, the egg is transformed into a proembryo and it has to be transferred to the uterus to continue its development. The first human pregnancy generated by ICS was carried out in 1991 by Gianpiero Palermo and his team. Round spermatid injection (ROSI) is a technique of assisted reproduction whereby a round spermatid is injected into oocyte cytoplasm in order to achieve fertilization. This technique can be used to enable genetic fatherhood to some men who have no spermatozoa in the ejaculate (azoospermia) and in whom spermatozoa cannot be obtained surgically from the testicles. This condition is called nonobstructive or secretory azoospermia, as opposed to obstructive azoospermia, in which complete sperm production does occur in the testicles, and potentially fertilizing spermatozoa can be obtained by testicular sperm extraction (TESE) and used for ICSI. In cases of nonobstructive (secretory) azoospermia, on the other hand, testicular sperm production is blocked at different stages of the process of sperm formation (spermatogenesis). In those men in whom spermatogenesis is blocked at the stage of round spermatids, in which meiosis has already been completed, these round cells can successfully fertilize oocytes after being injected into their cytoplasm. Before the development of the ROSI technique, men with the arrest of spermatogenesis at the round spermatid stage could only have children with the use of donor spermatozoa. Even though many technical aspects of ROSI are similar to those of ICSI, there are also significant differences between both techniques. In the first place, as compared to spermatozoa, round spermatids do not possess easily perceptible morphological characteristics and are immotile. Consequently, the distinction between round spermatids and other round cells of similar size, such as leukocytes, is not an easy task. Moreover, the distinction between living round spermatids, to be used in ROSI, and dead round spermatids, to be discarded, needs specific methods and skills, not required in the case of ICSI where sperm cell viability can be easily evaluated on the basis of sperm motility in most cases. The microinjection procedure for ROSI also differs slightly from that of ICSI, since additional stimuli are needed to ensure proper oocyte activation after spermatid injection. If all requirements for round spermatid selection and injection are successfully met, the injected oocytes develop to early embryos and can be transferred to the mother’s uterus to produce pregnancy. The first successful pregnancies and births with the use of ROSI were achieved in 1995 by Jan Tesarik and his team. The clinical potential of ROSI in the treatment of male infertility due to the total absence of spermatozoa has been corroborated recently by a publication reporting on the postnatal development of 90 babies born in Japan and 17 in Spain. Based on the evaluation of the babies born, no abnormalities attributable to the ROSI technique have been identified. This procedure is most commonly used to overcome male infertility problems, although it may also be used where eggs cannot easily be penetrated by sperm, and occasionally in addition to sperm donation. It can be used in teratozoospermia, because once the egg is fertilized, abnormal sperm morphology does not appear to influence blastocyst development or blastocyst morphology. Even with severe teratozoospermia, microscopy can still detect the few sperm cells that have a 'normal' morphology, allowing for optimal success rate.