Pap test

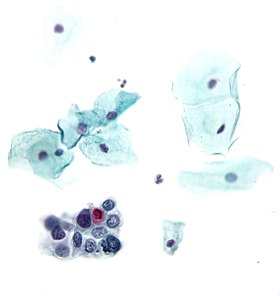
The Papanicolaou test (abbreviated as Pap test, also known as Pap smear, cervical smear, cervical screening or smear test) is a method of cervical screening used to detect potentially precancerous and cancerous processes in the cervix (opening of the uterus or womb). Abnormal findings are often followed up by more sensitive diagnostic procedures and if warranted, interventions that aim to prevent progression to cervical cancer. The test was independently invented in the 1920s by Dr. Georgios Papanikolaou and Dr. Aurel Babeș and named after Papanikolaou. A simplified version of the test was introduced by Anna Marion Hilliard in 1957.Micrograph of a normal pap smearMicrograph of a Pap test showing a low-grade intraepithelial lesion (LSIL) and benign endocervical mucosa. Pap stain.Micrograph of a Pap test showing trichomoniasis. Trichomonas organism seen in the upper right. Pap stain.Micrograph of a Pap test showing changes of herpes simplex virus. Pap stain.Endocervical adenocarcinoma on a pap test.Candida organisms on a pap test.Viral cytopathic effect consistent with herpes simplex virus on a pap test.Normal squamous epithelial cells in premenopausal womenAtrophic squamous cells in postmenopausal womenNormal endocervical cells should be present into the slide, as a proof of a good quality samplingthe cytoplasms of squamous epithelial cells melted out; many Döderlein bacilli can be seenInfestation by Trichomonas vaginalisAn obviously atypical cell can be seen The Papanicolaou test (abbreviated as Pap test, also known as Pap smear, cervical smear, cervical screening or smear test) is a method of cervical screening used to detect potentially precancerous and cancerous processes in the cervix (opening of the uterus or womb). Abnormal findings are often followed up by more sensitive diagnostic procedures and if warranted, interventions that aim to prevent progression to cervical cancer. The test was independently invented in the 1920s by Dr. Georgios Papanikolaou and Dr. Aurel Babeș and named after Papanikolaou. A simplified version of the test was introduced by Anna Marion Hilliard in 1957. A Pap smear is performed by opening the vaginal canal with a speculum and collecting cells at the outer opening of the cervix at the transformation zone (where the outer squamous cervical cells meet the inner glandular endocervical cells). The collected cells are examined under a microscope to look for abnormalities. The test aims to detect potentially precancerous changes (called cervical intraepithelial neoplasia (CIN) or cervical dysplasia; the squamous intraepithelial lesion system (SIL) is also used to describe abnormalities) caused by human papillomavirus, a sexually transmitted DNA virus. The test remains an effective, widely used method for early detection of precancer and cervical cancer. While the test may also detect infections and abnormalities in the endocervix and endometrium, it is not designed to do so. In the United States, Pap smear screening is recommended starting around 21 years of age until the age of 65. However, other countries do not recommend pap testing in non-sexually active females. Guidelines on frequency vary from every three to five years. If results are abnormal, and depending on the nature of the abnormality, the test may need to be repeated in six to twelve months. If the abnormality requires closer scrutiny, the patient may be referred for detailed inspection of the cervix by colposcopy. The person may also be referred for HPV DNA testing, which can serve as an adjunct to Pap testing. Additional biomarkers that may be applied as ancillary tests with the Pap test are evolving. Screening guidelines vary from country to country. In general, screening starts about the age of 20 or 25 and continues until about the age of 50 or 60. Screening is typically recommended every three to five years, as long as results are normal. Women should wait a few years after they first have intercourse before they start screening, and should not be screened before age 21. American Congress of Obstetricians and Gynecologists (ACOG) and others recommend starting screening at age 21 (since that is a few years after sexual debut for most American women). Many other countries wait until age 25 or later to start screening. For instance, some parts of Great Britain start screening at age 25. ACOG's general recommendation is that people with female reproductive organs age 30–65 have an annual well-woman examination, that they not get annual Pap tests, and that they do get Pap tests at three-year intervals. HPV is passed through skin to skin contact; sex does not have to occur, although it is a common way for it to spread. It takes an average of a year, but can take up to four years, for a person's immune system to control the initial infection. Screening during this period may show this immune reaction and repair as mild abnormalities, which are usually not associated with cervical cancer, but could cause the patient stress and result in further tests and possible treatment. Cervical cancer usually takes time to develop, so delaying the start of screening a few years poses little risk of missing a potentially precancerous lesion. For instance, screening people under age 25 does not decrease cancer rates under age 30. There is little or no benefit to screening people who have not had sexual contact. For example, United States Preventive Services Task Force (USPSTF) recommends waiting at least three years after first sex. HPV can be transmitted in sex between females, so those who have only had sex with other females should be screened, although they are at somewhat lower risk for cervical cancer. Guidelines on frequency of screening vary—typically every three to five years for those who have not had previous abnormal smears. Some older recommendations suggested screening as frequently as every one to two years, however there is little evidence to support such frequent screening; annual screening has little benefit but leads to greatly increased cost and many unnecessary procedures and treatments. It has been acknowledged since before 1980 that most people can be screened less often. In some guidelines, frequency depends on age; for instance in Great Britain, screening is recommended every 3 years for women under 50, and every 5 years for those over. Screening should stop at about age 65 unless there is a recent abnormal test result or disease. There is probably no benefit in screening people aged 60 or over whose previous tests have been negative. If a woman's last three Pap results were normal, she can discontinue testing at age 65, according to the USPSTF, ACOG, ACS and ASCP; England's NHS says 64.There is no need to continue screening after a complete hysterectomy for benign disease.