Androgen deprivation therapy

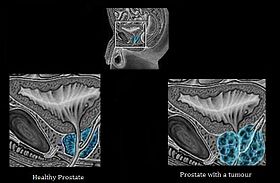
Androgen deprivation therapy (ADT), also called androgen suppression therapy, is an antihormone therapy whose main use is in treating prostate cancer. Prostate cancer cells usually require androgen hormones, such as testosterone, to grow. ADT reduces the levels of androgen hormones, with drugs or surgery, to prevent the prostate cancer cells from growing. The pharmaceutical approaches include antiandrogens and chemical castration. Androgen deprivation therapy (ADT), also called androgen suppression therapy, is an antihormone therapy whose main use is in treating prostate cancer. Prostate cancer cells usually require androgen hormones, such as testosterone, to grow. ADT reduces the levels of androgen hormones, with drugs or surgery, to prevent the prostate cancer cells from growing. The pharmaceutical approaches include antiandrogens and chemical castration. Several studies have concluded that ADT has demonstrated benefit in patients with metastatic disease, and as an adjunct to radiation therapy in patients with locally advanced disease, as well as those with unfavorable intermediate-risk or high-risk localized disease. However, in patients with low-risk prostate cancer, ADT has demonstrated no survival advantage, and significant harm, such as impotence, diabetes and bone loss. The therapy can also eliminate cancer cells by inducing androgen deprivation-induced senescence. Lowering androgen levels or stopping them from getting into prostate cancer cells often makes prostate cancer shrink or grow more slowly for a time. However, this treatment needs to be combined with radiation therapy (RT) because ADT itself does not eradicate the cancer; it just decreases its aggressiveness. The synthesis of testosterone is mediated by a chain of processes that start in our brain. When our body detects a low level of testosterone, the hypothalamus starts to produce LHRH, a hormone which, once is received by the pituitary gland activates the synthesis of LH (Luteinizing hormone). LH travels to the testicles where it induces the formation of testosterone.There are two methods of androgen deprivation therapy based on drugs. One works preventing the pituitary gland from releasing LH and the other one blocks the body’s ability to use androgens. Normal male sexuality seems to depend upon very specific and complicated hormonal patterns that are not completely understood. One study suggests that ADT can alter the hormonal balance necessary for male sexual activity. As men age, testosterone levels decrease by about 1% a year after age 30; however, it is important to determine whether low testosterone is due to normal aging, or to a disease, such as hypogonadism. Testosterone plays a significant role in sexual functioning; therefore, naturally declining levels of testosterone can lead to reduction in normal sexual functioning. Further decreases in serum testosterone can have a negative impact on normal sexual function, leading to a decline in quality of life. Erectile dysfunction is not uncommon after radical prostatectomy and men who undergo ADT in addition to this are likely to show further decline in their ability to engage in penetrative intercourse, as well as their desire to do so. A study looking at the differences of using GnRH-A (and androgen suppressant) or an orchiectomy report differences in sexual interest, the experience of erections, and the prevalence of participating in sexual activity. Men reporting no sexual interest increased from 27.6% to 63.6% after orchiectomy, and from 31.7% to 58.0% after GnRH-A; men who experienced no erections increased from 35.0% to 78.6%; and men who did not report engaging in sexual activity increased from 47.9% to 82.8% after orchiectomy and 45.0% to 80.2%. This study suggests that the GnRH-A and orchiectomy had similar effects on sexual functioning. A vicious cycle whereby lowering testosterone levels leads to decreased sexual activity, which in turn cause both free and total testosterone levels to decline even further. This demonstrates the importance of androgens for maintaining sexual structures and functions. Although targeting the androgen axis has clear therapeutic benefit, its effectiveness is temporary, as prostate tumor cells adapt to survive and grow. The removal of androgens has been shown to activate epithelial–mesenchymal transition (EMT), neuroendocrine transdifferentiation (NEtD) and cancer stem cell-like gene programs. Thus, activation of these programs via inhibition of the androgen axis provides a mechanism by which tumor cells can adapt to promote disease recurrence and progression. Orchiectomy, LHRH analogs and LHRH antagonists can all cause similar side effects, due to changes in the levels of sex hormones (testosterone).