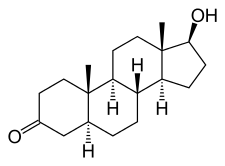
Dihydrotestosterone

Dihydrotestosterone (DHT, 5α-dihydrotestosterone, 5α-DHT, androstanolone or stanolone) is an endogenous androgen sex steroid and hormone. The enzyme 5α-reductase catalyzes the formation of DHT from testosterone in certain tissues including the prostate gland, seminal vesicles, epididymides, skin, hair follicles, liver, and brain. This enzyme mediates reduction of the C4-5 double bond of testosterone. Relative to testosterone, DHT is considerably more potent as an agonist of the androgen receptor (AR). Dihydrotestosterone (DHT, 5α-dihydrotestosterone, 5α-DHT, androstanolone or stanolone) is an endogenous androgen sex steroid and hormone. The enzyme 5α-reductase catalyzes the formation of DHT from testosterone in certain tissues including the prostate gland, seminal vesicles, epididymides, skin, hair follicles, liver, and brain. This enzyme mediates reduction of the C4-5 double bond of testosterone. Relative to testosterone, DHT is considerably more potent as an agonist of the androgen receptor (AR). In addition to its role as a natural hormone, DHT has been used as a medication, for instance in the treatment of low testosterone levels in men; for information on DHT as a medication, see the androstanolone article. DHT is biologically important for sexual differentiation of the male genitalia during embryogenesis, maturation of the penis and scrotum at puberty, growth of facial, body, and pubic hair, and development and maintenance of the prostate gland and seminal vesicles. It is produced from the less potent testosterone by the enzyme 5α-reductase in select tissues, and is the primary androgen in the genitals, prostate gland, seminal vesicles, skin, and hair follicles. DHT signals mainly in an intracrine and paracrine manner in the tissues in which it is produced, playing only a minor role, if any, as a circulating endocrine hormone. Circulating levels of DHT are 1/10th and 1/20th those of testosterone in terms of total and free concentrations, respectively, whereas local DHT levels may be up to 10 times those of testosterone in tissues with high 5α-reductase expression such as the prostate gland. In addition, unlike testosterone, DHT is inactivated by 3α-hydroxysteroid dehydrogenase (3α-HSD) into the very weak androgen 3α-androstanediol in various tissues such as muscle, adipose, and liver among others, and in relation to this, DHT has been reported to be a very poor anabolic agent when administered exogenously as a medication. In addition to normal biological functions, DHT also plays an important causative role in a number of androgen-dependent conditions including hair conditions like hirsutism (excessive facial/body hair growth) and pattern hair loss (androgenic alopecia or pattern baldness) and prostate diseases such as benign prostatic hyperplasia (BPH) and prostate cancer. 5α-Reductase inhibitors, which prevent DHT synthesis, are effective in the prevention and treatment of these conditions. Metabolites of DHT have been found to act as neurosteroids with their own AR-independent biological activity. 3α-Androstanediol is a potent positive allosteric modulator of the GABAA receptor, while 3β-androstanediol is a potent and selective agonist of the estrogen receptor (ER) subtype ERβ. These metabolites may play important roles in the central effects of DHT and by extension testosterone, including their antidepressant, anxiolytic, rewarding/hedonic, anti-stress, and pro-cognitive effects. Much of the biological role of DHT has been elucidated in studies of individuals with congenital 5α-reductase type II deficiency, an intersex condition caused by a loss-of-function mutation in the gene encoding 5α-reductase type II, the major enzyme responsible for the production of DHT in the body. It is characterized by a defective and non-functional 5α-reductase type II enzyme and a partial but majority loss of DHT production in the body. In the condition, circulating testosterone levels are within or slightly above the normal male range, but DHT levels are low (around 30% of normal), and the ratio of circulating testosterone to DHT is greatly elevated (at about 3.5 to 5 times higher than normal). Genetic males (46,XY) with 5α-reductase type II deficiency are born with undervirilization including pseudohermaphroditism (ambiguous genitalia), pseudovaginal perineoscrotal hypospadias, and usually undescended testes. Their external genitalia are female-like, with micropenis (a small, clitoris-like phallus), a partially unfused, labia-like scrotum, and a blind-ending, shallow vaginal pouch. Due to their lack of conspicuous male genitalia, genetic males with the condition are typically raised as girls. At the time of puberty however, they develop striking phenotypically masculine secondary sexual characteristics including partial virilization of the genitals (enlargement of the phallus into a near-functional penis and descent of the testes), voice deepening, typical male musculoskeletal development, and no menstruation, breast development, or other signs of feminization that occur during female puberty. In addition, normal libido and spontaneous erections develop, they usually show a sexual preference for females, and almost all develop a male gender identity. Nonetheless, males with 5α-reductase type II deficiency exhibit signs of continued undervirilization in a number of domains. Facial hair was absent or sparse in a relatively large group of Dominican males with the condition, known as the Güevedoces. However, more facial hair has been observed in patients with the disorder from other parts of the world, although facial hair was still reduced relative to that of other men in the same communities. The divergent findings may reflect racial differences in androgen-dependent hair growth. A female pattern of androgenic hair growth, with terminal hair largely restricted to the axillae and lower pubic triangle, is observed in males with the condition. No temporal recession of the hairline or androgenic alopecia (pattern hair loss or baldness) has been observed in any of the cases of 5α-reductase type II deficiency that have been reported, whereas this is normally seen to some degree in almost all Caucasian males. Individuals with 5α-reductase type II deficiency were initially reported to have no incidence of acne, but subsequent research indicated normal sebum secretion and acne incidence.