Heart transplantation

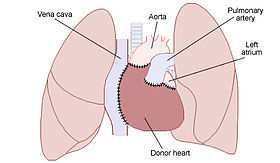
A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2018, the most common procedure is to take a functioning heart, with or without transplanting one or both lungs at the same time, from a recently deceased organ donor (brain death is the standard) and implanting it into the patient. The patient's own heart is either removed and replaced with the donor heart (orthotopic procedure) or, much less commonly, the recipient's diseased heart is left in place to support the donor heart (heterotopic, or 'piggyback', transplant procedure). A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2018, the most common procedure is to take a functioning heart, with or without transplanting one or both lungs at the same time, from a recently deceased organ donor (brain death is the standard) and implanting it into the patient. The patient's own heart is either removed and replaced with the donor heart (orthotopic procedure) or, much less commonly, the recipient's diseased heart is left in place to support the donor heart (heterotopic, or 'piggyback', transplant procedure). Approximately 3,500 heart transplants are performed every year in the world, more than half of which occur in the US. Post-operation survival periods average 15 years. Heart transplantation is not considered to be a cure for heart disease; with that being said, it still is a life-saving treatment intended to improve the quality, and hopefully also both the overall total duration of time and the extent of time afterwards in a more active state, of life for the recipients. One of the first mentions of the possibility of heart transplantation was by American medical researcher Simon Flexner, who declared in a reading of his paper on 'Tendencies in Pathology' in the University of Chicago in 1907 that it would be possible in the then-future for diseased human organs substitution for healthy ones by surgery — including arteries, stomach, kidneys and heart. Not having a human donor heart available, James D. Hardy of the University of Mississippi Medical Center transplanted the heart of a chimpanzee into the chest of a dying Boyd Rush in the early morning of Jan. 24, 1964. Hardy used a defibrillator to shock the heart to restart beating. This heart did beat in Rush's chest for 60 to 90 minutes (sources differ), and then Rush died without regaining consciousness. Although Hardy was a respected surgeon who had performed the world's first human-to-human lung transplant a year earlier, author Donald McRae states that Hardy could feel the 'icy disdain' from fellow surgeons at the Sixth International Transplantation Conference several weeks after this attempt with the chimpanzee heart. Hardy had been inspired by the limited success of Keith Reemtsma at Tulane University in transplanting chimpanzee kidneys into human patients with kidney failure. The consent form Hardy asked Rush's step sister to sign did not include the possibility that a chimpanzee heart might be used, although Hardy stated that he did include this in verbal discussions. A xenotransplantation is the technical term for the transplant of an organ or tissue from one species to another. The world's first human-to-human heart transplant was performed by South African cardiac surgeon Christiaan Barnard utilizing the techniques developed by American surgeons Norman Shumway and Richard Lower. Patient Louis Washkansky received this transplant on December 3, 1967, at the Groote Schuur Hospital in Cape Town, South Africa. Washkansky, however, died 18 days later from pneumonia. On December 6, 1967, at Maimonides Hospital in Brooklyn, New York, Adrian Kantrowitz performed the world's first pediatric heart transplant. The infant's new heart stopped beating after 7 hours and could not be restarted. At a following press conference, Kantrowitz emphasized that he did not consider the operation a success. Norman Shumway performed the first adult heart transplant in the United States on January 6, 1968, at the Stanford University Hospital. A team led by Donald Ross performed the first heart transplant in the United Kingdom on May 3, 1968. These were allotransplants, the technical term for a transplant from a non-genetically identical individual of the same species. Brain death is the current ethical standard for when a heart donation can be allowed. Worldwide, more than 100 transplants were performed by various doctors during 1968. Only a third of these patients lived longer than three months. The next big breakthrough came in 1983 when cyclosporine entered widespread usage. This drug enabled much smaller amounts of corticosteroids to be used to prevent many cases of rejection (the 'corticosteroid-sparing' effect of cyclosporine).